Alzheimer’s disease, the most common form of dementia, may be influenced by factors circulating in the blood. In mouse experiments, blood from aged animals accelerated amyloid plaque buildup and cognitive decline, while young blood showed protective effects. Credit: Shutterstock
A new study shows that components found in aged blood can speed up the buildup of amyloid proteins and alter behavior in an experimental mouse model of Alzheimer’s disease.
Alzheimer’s disease is the leading cause of dementia worldwide and remains a major challenge for public health systems. A new study published in the journal Aging reports that blood taken from older mice can speed up the progression of Alzheimer’s-related changes, while blood from younger mice appears to offer protective benefits.
The research was conducted by scientists from Instituto Latinoamericano de Salud Cerebral (BrainLat) at Universidad Adolfo Ibáñez, working alongside colleagues from MELISA Institute, the University of Texas Health Science Center at Houston, and Universidad Mayor.
The disease is marked by the buildup of beta-amyloid protein (Aβ) in the brain. These protein deposits form plaques that interfere with communication between nerve cells and drive the processes that lead to neurodegeneration. While beta-amyloid is produced in the central nervous system, growing evidence suggests that it can also be found in the bloodstream, raising new questions about how Alzheimer’s develops and spreads.
Testing How Age-Related Blood Factors Affect the Brain
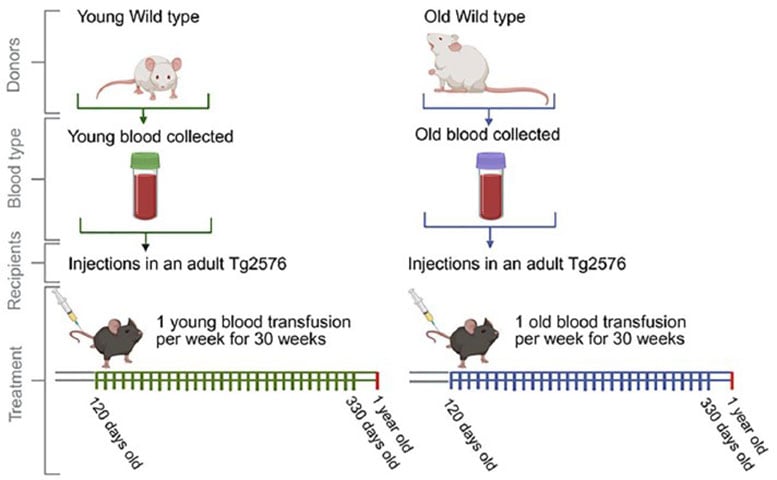
To investigate the role of age-related factors in blood, the researchers turned to Tg2576 transgenic mice (a model widely used in Alzheimer’s research). Over a 30-week period, these mice received weekly blood infusions from either young or aged animals. The goal was to determine whether substances circulating in the blood could influence amyloid plaque buildup in the brain as well as changes in behavior.
Schematic representation of the blood infusion regime (blood from old and young wild type mice into Tg2576 mice). Wild-type mice aged 50–75 days (WT Young mice), and wild-type mice aged 443–532 days (WT Old mice) served as blood donors. This blood was transfused to 120-day-old Tg2576 mice, which then underwent to weekly transfusions and sacrificed at 363–366 days old. Before sacrificing, mice were evaluated for spatial memory.
Postmortem analyses included immunopathological, biochemical, and proteomic evaluations of brain tissues. Credit: Aging
“This collaborative work between various institutions reinforces the importance of understanding how systemic factors condition the brain environment and directly impact mechanisms that promote disease progression. By demonstrating that peripheral signals derived from aged blood can modulate central processes in the pathophysiology of Alzheimer’s, these findings open new opportunities to study therapeutic targets aimed at the blood-brain axis,” explained Dr.
Claudia Durán-Aniotz, from the Instituto Latinoamericano de Salud Cerebral (BrainLat) at Universidad Adolfo Ibáñez.
Measuring Memory, Plaques, and Protein Changes
The team assessed cognitive performance using the Barnes test, the accumulation of amyloid plaques with histological and biochemical techniques, and performed a comprehensive proteomic analysis of the treated brains. This analysis revealed more than 250 differentially expressed proteins, linked to synaptic functions, endocannabinoid signaling, and calcium channels, which could explain the observed changes.
Regarding MELISA Institute’s participation in this research, Mauricio Hernández, a proteomics expert at the research and biotechnology center, commented that “within this study, we conducted a large-scale proteomic analysis that allowed us to generate excellent quality data in this complex matrix like plasma, a technical challenge for any proteomics laboratory. Thanks to our state-of-the-art equipment (timsTOF Pro2), we are proud to have contributed to the production of a robust and high-quality scientific article.”
What the Findings Suggest and What Comes Next
These results reinforce the idea that circulating factors in the blood can directly influence the progression of neurodegenerative diseases such as Alzheimer’s. Understanding these mechanisms will allow for the identification of new therapeutic targets and preventative strategies. The next step will be to determine exactly what these factors are and whether it is possible to intervene in them in humans.
“It is a pleasure to contribute our proteomic capabilities to support innovative research initiatives like this study, which allow us to advance the knowledge and development of new therapies for neurodegenerative diseases, which are currently a global health problem,” emphasized Dr. Elard Koch, Chairman of MELISA Institute.
Reference: “Infusion of blood from young and old mice modulates amyloid pathology” by Matias Pizarro, Ruben Gomez-Gutierrez, Ariel Caviedes, Catalina Valdes, Ute Woehlbier, Cristian Vargas, Mauricio Hernandez, Claudia Duran-Aniotz and Rodrigo Morales, 12 September 2025, Aging.
was supported by ANID/FONDECYT Regular 1210622, ANID/PIA/ANILLOS ACT210096, the Alzheimer’s Association (AARGD-24-1310017), ANID/FOVI240065 and ANID/Proyecto Exploracion 13240170 and MULTI-PARTNER CONSORTIUM TO EXPAND DEMENTIA RESEARCH IN LATIN AMERICA (ReDLat), supported by NIH research grant R01AG057234 funded by the National Institute of Aging (NIA) and the Fogarty International Center (FIC), an Alzheimer’s Association grant (SG-20-725707-ReDLat), the Rainwater Charitable Foundation, and the Global Brain Health Institute with additional support from the Bluefield Project to Cure Frontotemporal Dementia, an NIH contract (75NS95022C00031), and NIA under awards R01AG075775, R01AG082056, and R01AG083799. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health, the Alzheimer’s Association, Rainwater Charitable Foundation, Bluefield Project to Cure Frontotemporal Dementia, or the Global Brain Health Institute.
The contribution of RM and team in this work was supported by NIH grants RF1AG072491 and RF1AG059321. UW was supported by ANID/FONDECYT Regular 1240176.
Never miss a breakthrough: Join the SciTechDaily newsletter.
Follow us on Google and Google News.






Comments(0)
Join the conversation and share your perspective.
Sign In to Comment